The discovery of the Papillon-Lefèvre syndrome, a rare cathepsin C related lysosomal disease
From the perspective of unmet medical needs, drug repurposing for rare diseases offers a great opportunity. There are more than 7000 rare diseases, and over 95% of them lack an approved therapeutic agent, but new drug development for specific rare diseases is not a priority for the pharmaceutical industry. Drug repositioning would be a particularly attractive approach for rare diseases for both scientific and commercial reasons. Two special issues on the topic: “Cathepsin C and Neutrophil serine proteases in rare diseases” for Rare Disease and Orphan Drugs Journal resulted from the 3rd International Symposium on Cathepsin C, IsyCatC III (Tours/France, April 2022) organized in memory of Dr. Paul Henri Papillon & Dr. Paul Philippe Henri Lefèvre.
The International Cathepsin-C Consortium (ICat-CC) was set up in 2016 thanks to the collaboration of world’s leading specialists from academic labs and industry, working on lysosomal cysteine protease cathepsin C (CatC) [also known as dipeptidypeptidase 1 (DPP1)] and its target proteases including neutrophil serine proteases (NSPs, elastase, proteinase 3, cathepsin G and NSP4). Inflammation-mediated immune cell alterations are associated with many diseases, including acute and chronic inflammatory diseases and cancer. There is an unmet need for new therapies that go beyond symptomatic relief and temporary interruption of disease progression. NSPs are locally released in response to pathogens and many other non-infectious danger signals. Uncontrolled NSPs are involved in neutrophil-mediated inflammatory diseases and are considered as important therapeutic targets. CatC attracts more and more attention from both scientists and clinicians because of its role in the activation of pro-inflammatory NSPs implicated in certain chronic inflammatory/auto-immune disorders. Promising preclinical and clinical data suggest that pharmacological inhibition of NSPs might ameliorate these conditions.
Papillon-Lefèvre syndrome (PLS) is a rare autosomal recessive trait caused by mutations in the CTSC gene which encodes CatC[1-3]. Patients with PLS have a genetically determined deficiency in CatC but, reassuringly, do not exhibit marked immunodeficiency despite the absence of NSPs in immune defense cells. Hence, the pharmacological control of CatC activity in bone marrow precursor cells represents an attractive therapeutic strategy for neutrophil serine protease-mediated disorders. A variety of CatC inhibitors, developed by pharmaceutical companies and academic investigators, are currently being evaluated in preclinical/clinical trials as anti-inflammatory drugs. An invited review article on the therapeutic targeting of CatC resulted from the first International Symposium on Cathepsin C IsyCatC (Tours/France, April 2017) and was published in the journal Pharmacology and Therapeutics[3].
A CatC inhibitor is currently being tested in Phase 3 in patients with bronchiectasis, a chronic inflammatory lung disease defined by permanent dilatation of the bronchi. This development is very encouraging for biochemists studying the functionality of CatC, cell biologists studying its maturation and tissue localization, chemists developing specific CatC inhibitors and clinicians managing patients with NSPs-mediated disorders. Due to overlapping phenotypes and similar underpinning molecular mechanisms for several inflammatory diseases, a positive effect in bronchiectasis could be translated directly to the potential treatment of other NSPs-mediated inflammatory diseases. It is gratifying to see that the hard work of all colleagues from academic labs and industry and advocacy in the CatC field may have a clinical payoff.
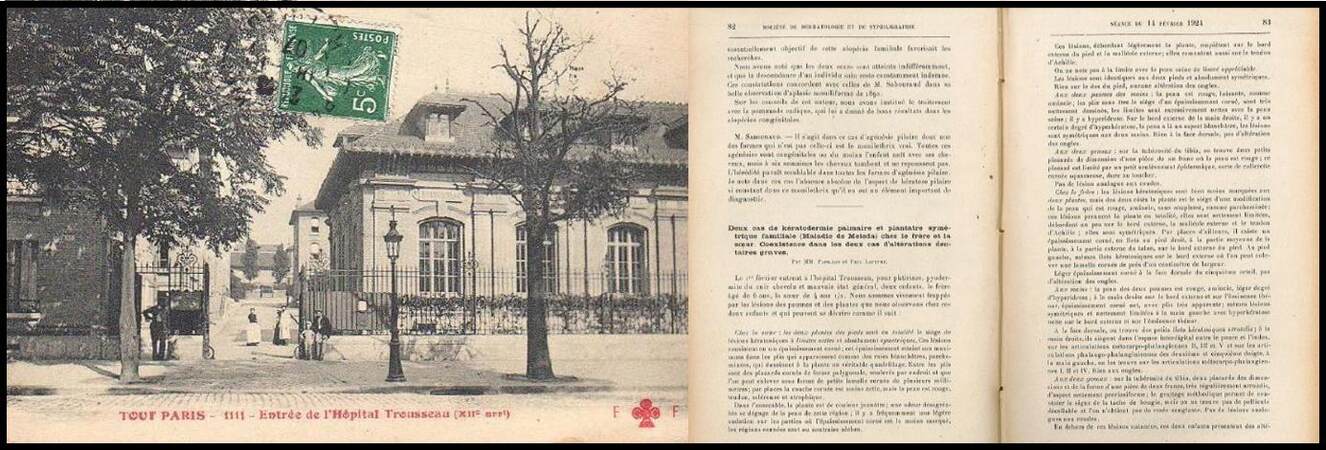
In 1924, two French physicians, Paul Henri Papillon (1866-1945) and Paul Philippe Henri Lefèvre (1891-1982), working at the Armand Trousseau Children’s Hospital in Paris, observed severe lesions on the palms and soles of two siblings with extensive dental decay. The coexistence of palmoplantar keratoderma with dental decay was novel and highlighted in the article they published on February 14, 1924, in French, in Bull Soc Fr Dermatol Syph, 1924;31:82-7[4] [Figure 1]. The disease characterized by these symptoms was named “Papillon-Lefèvre syndrome” (PLS) after the 1960s and is characterized by severe periodontitis and palmoplantar keratoderma developing between the first and fifth years of life, with subsequent loss of teeth[1,2]. We present in this Editorial the initial article describing the first patients with biographical information about Dr. Papillon and Dr. Lefèvre, including unpublished pictures from the archives.
Figure 1. Exterior view of the main entrance to Armand Trousseau Children’s Hospital printed on a postcard (left) and the first pages of the initial 1924 article (right).
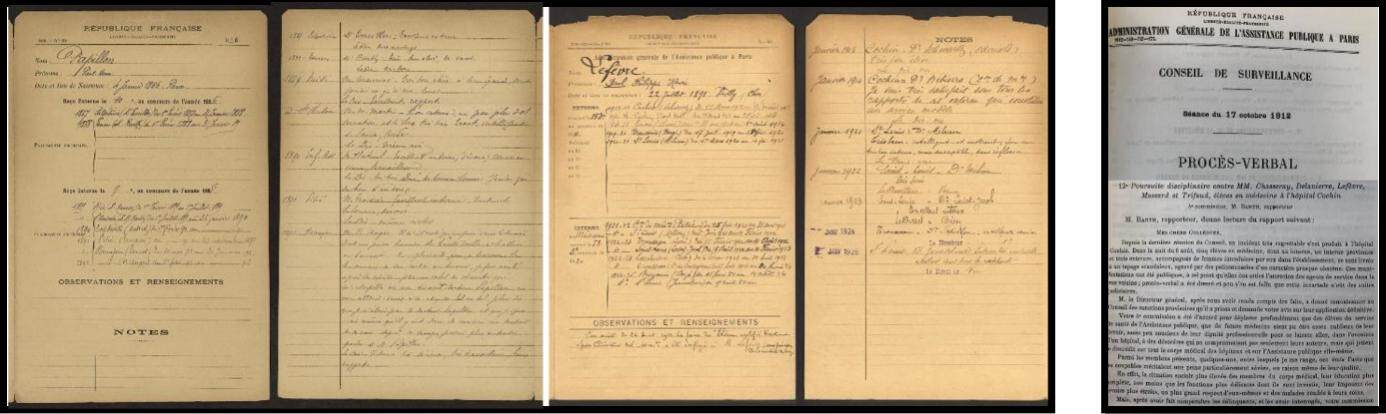
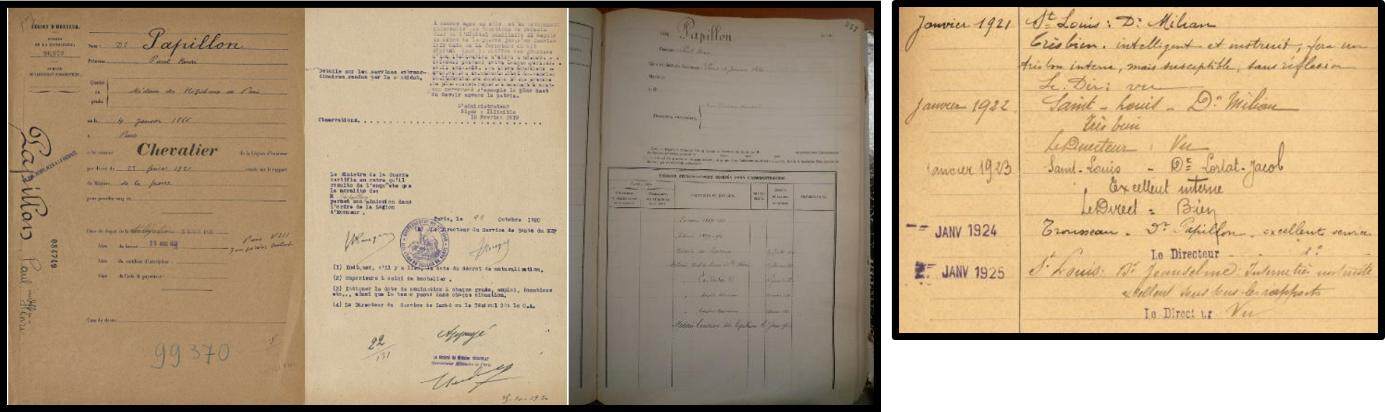
Paul Henri Papillon, son of Louis Alexandre Papillon and Pauline Suzanne Papillon, was born in Paris, in the city’s 1st arrondissement, on January 4, 1866. His father was a grocer and his mother was a housewife. In 1896, he married Marguerite Coulbaux (1873-1906), with whom he had a son, Jacques Papillon (1899-1984). Paul Henri Papillon graduated from the Paris School of Medicine and completed internships between 1889 and 1892. His thesis for the doctorate in medicine entitled « Study of histological lesions of the liver and kidneys in cholera (Beaujon epidemic 1892) » was published in 1893. He was a paediatrician and was appointed head of department at Sainte Périne Hospital, Paris on February 1, 1911 [Figure 2]. He worked as head of Auxiliary Hospital 31 at Levallois Perret during the 1st world war, where his service earned him in 1921 the highest French honour for military and civil merit awarded by the French Ministry of War, Knight of the Legion of Honour for his professionalism as a physician during the world war [Figure 3]. He completed 14 years of service as a physician in Paris Hospitals [Figures 4 and 5]. He was appointed head of the infectious disease department in Armand Trousseau Children’s Hospital in Paris on February 1, 1921, where he met Dr Lefèvre. He died on May 30, 1945, in the house where he was born, 7 Frederic Bastiat. The death certificate was signed by the local liberation committee representative.
Figure 2. School certificates of Dr. Papillon and Dr. Lefèvre (left) and minutes of disciplinary prosecution against five medical students including Lefèvre (right).
Figure 3. Certificate of appointment to « Chevalier de la Légion d’Honneur » of Dr. Papillon with his career certificate (left) and his appreciation regarding his junior assistant Lefèvre (right).
Figure 4. Photos of the staff of Dr. Papillon’s service and that of Dr. Lesné (Trousseau Hospital, 1922).
Figure 5. Photos of the staff of Dr. Papillon’s service (left, Trousseau Hospital, 1931) and that of Dr. Lartot-Jacob (Saint Louis Hospital, 1925). Dr. Papillon seated in the middle of the first row (left) and Dr. Lefèvre at the end of the first row.
Paul Henri Philippe Lefèvre, son of Louis Marie Clair Henry Lefèvre and Marie Louise Henriette Lefèvre, was born in Vailly-sur-Sauldre (Cher, Centre-Val de Loire, France) on July 23, 1891. His father was a physician and his mother was a housewife. As a student, Lefèvre was stripped of his bronze medal and nearly thrown out of his medical school because of a regrettable incident on hospital premises involving drunkenness and young ladies during the night of August 6, 1912 [Figure 3]. He graduated in 1921 as a dermatologist. He completed internships between 1921 and 1925 at Saint Louis and Trousseau hospitals. His thesis for the doctorate in medicine was entitled « Biological reactivation of the Bordet-Wassermann reaction (Milian’s method). His practice in the research of hereditary syphilis » was published in 1925. He was assistant to Dr. Papillon between August 15, 1923 and February 14, 1924. He died on June 30, 1982 in Beauvais (Oise, Hauts-de-France, France).
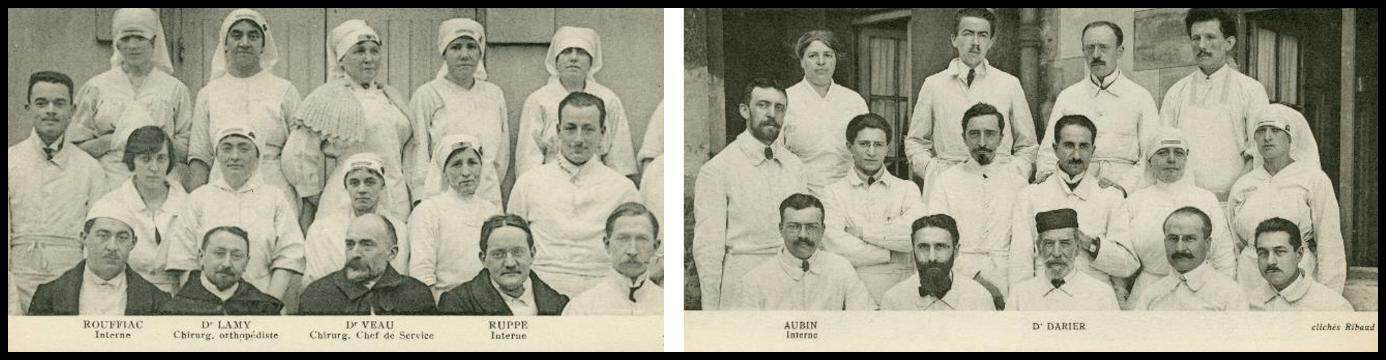
Dr. Papillon and Dr. Lefèvre published the first cases of PLS in 1924[4]. They examined a six-year-old boy and his four-and-a-half-year-old sister from Ulm (Germany), who presented at the Armand Trousseau Children Hospital in Paris on February 1, 1924. Their parents were first cousins. Dr. Papillon and his assistant Dr. Lefèvre observed striking lesions on the palms and soles as well as severe dental decay, which was described in detail by Dr. Ruppé (Enfants-Assistés Hospital, Paris). Dr. Darier (Saint-Louis Hospital, Paris) [Figure 6], internationally known as the doyen of French dermatology, agreed with the diagnosis of palmoplantar keratoderma analogous to that previously observed by E. Ehlers on the Island of Mljet (Meleda), Croatia (Mal de Meleda). However, the association of palmoplantar keratoderma with dental decay was novel and highlighted in the article translated into English below. Dr. Petges and Dr. Delguel presented a similar case in Bordeaux in 1927, apparently unaware of the communication from Papillon and Lefèvre.
Figure 6. Photos of the staff of Dr. Veau’s service (left, Enfants Assistés Hospital, 1922) and that of Dr. Darier (Saint Louis Hospital, 1922). Dr. Ruppe seated in the first row (left).
In 1951 Dr. Bataille, Paris Hospital stomatologist, presented another child with palmo-plantar keratoderma, in whom he followed progressive alveolar loss over several months. In 1954, E. Bélanger reported in his doctoral thesis the recessive character of “Papillon-Lefèvre type syndrome” or “Papillon-Lefèvre form” referring to Mal de Meleda keratoderma. Bélanger failed to locate the original patients described by Papillon and Lefèvre. It is historically interesting that the names and ethnicity of the children were not mentioned in the 1924 paper and they may have been deliberately concealed at that time. Only two years earlier, Dr. Papillon presented papers at the Paris Pediatric Society which did include patient names.
Two cases of familial symmetrical palmar and plantar keratoderma (Meleda’s disease) in a brother and sister. Coexistence in the two cases of serious dental abnormalities, by Messieurs PAPILLON and PAUL LEFEVRE
On February 1 two children, a boy aged six and his sister aged four-and-a-half, were admitted to Trousseau hospital with lice infestation, pyoderma of the scalp and poor general condition. We are struck by the lesions on the palms and soles of both children, which can be described as follows:
In the sister: the soles of both feet are entirely covered by symmetrical keratotic lesions with a distinct border. These lesions consist of a scaly thickening, maximal in the creases which look like whitish lines of parchment in a grid-like pattern. Between the creases are polygonal horny plaques, raised in places, which can be removed as small scales several millimeters across; in places, the horny layer is less prominent, but the skin is red, tense, hard and atrophic.
The sole is generally yellowish in color and an unpleasant odor emerges from the skin of this region; there is some perspiration in the less thickened areas; by contrast, the scaly regions are dry.
These lesions involving the sole encroach onto the side of the foot and the external malleolus and extend onto the Achilles tendon.
We do not observe any appreciable ridge at the junction with healthy skin.
The lesions are identical on both feet and absolutely symmetrical.
Nothing on the dorsum of the foot, no abnormality of the nails.
On both palms: the skin is red and shiny, as if thinned; the creases, lacking hyperkeratosis, are very distinct; the junction with healthy skin is excessively sharp; there is hyperhidrosis. On the outer edge of the right hand, there is a certain degree of hyperkeratosis, the skin has a whitish appearance, and the lesions are symmetrical on both hands. Nothing on the dorsal side, and no abnormality of the nails.
On both knees: on the tibial tuberosity there are two small plaques, the size of a one-franc piece, where the skin is red; this plaque has a slightly raised epidermal border, a sort of scaly collarette, hard to the touch.
No similar lesions on the elbow.
In the brother: the keratotic lesions on the soles are much less marked, but on both sides, there is a change in the plantar skin which is red, atrophic and stiff like parchment; these lesions cover the whole plantar surface with a clear border, extending a little over the outer edge, the lateral malleolus and the Achilles tendon; they are symmetrical. Also, there are islands of epidermal thickening on the right foot, in the middle of the sole, on the outer part of the heel and on the outer edge of the foot. On the left foot, the same keratotic islets occur on the outer edge, where you can remove a lamellar scale almost one centimeter wide.
Slight scaly thickening on the dorsal surface of the fifth toe, but no nail changes.
On the hands: the skin of both palms is red, thinned with mild hyperhidrosis; on the right hand there is distinct epidermal thickening, with very visible creases on the outer edge and on the thenar eminence; this is symmetrical with clearly demarcated lesions on the left hand with discrete hyperkeratosis on the outer edge and on the thenar eminence.
On the dorsal surface, there are small round scaly patches; on the right hand, they are situated in the thumb web, over the second, third and fifth metacarpo-phalangeal joints and over the interphalangeal joints of the second and fifth fingers. On the left hand, they are found over the first, second and fourth metacarpo-phalangeal joints. Nothing on the nails.
On both knees: on the tibial tuberosities are two round plaques of the size and shape of a two-franc piece with a distinctly psoriasiform appearance; scraping reveals the “candle-wax sign” as seen in psoriasis, but there is no detachable scale or pinpoint bleeding. No similar lesions on the elbow.
Besides these skin lesions, these two children have extensive dental abnormalities that Mr. Ruppe has kindly described to us.
The boy is completely edentulous, and resorption of the alveolar ridge is, like in adults, at the expense of the external cortical bone plate for the upper jaw and at the expense of the internal cortical bone plate for the lower jaw; so that the upper arch represented by the alveolar crest is actually imprinted in the lower arch. The upper lip is retracted and the child looks very much like a toothless old woman. When palpating the vestibular region, above the alveolar ridge, one feels the protrusion of the permanent dental follicles; the eruption of the first molars is already over.
The girl retains her lower right lateral incisor, her lower right canine, her second right deciduous molar , left lower lateral incisor, canine and second lower left molars, lateral incisor, canine, second right upper deciduous molar, canine and two left upper deciduous molars; the impression given by these teeth, many of which are decayed, is of a process of alveolar dental pyorrhea; the canines are exposed to a greater or lesser extent, they are set in a fungating red mucosa and the teeth are loose.
The boy weighs 14.85 kg at 6 years old, which is below the normal weight for his age, and he is thin and pale and in poor general condition. On the skin, in addition to the lesions mentioned above, he has pyoderma of the left outer ear, and numerous plaques of cicatricial alopecia, secondary to impetigo.
There is very marked lymphadenopathy: cervical nodes, especially on the right, one of which has suppurated as evidenced by a scar, bilateral submaxillary nodes, and small and mobile inguinal nodes. In the left inguinal crease, there is a scar from a suppurating lymph node, brownish at the edges, depigmented in the center, and elongated parallel to and below the inguinal ligament. No epitrochlear lymph nodes.
Examination of the lungs reveals nothing abnormal, other than a few bronchitic rattles.
However, radiological examination showed complete opacity of the left lung, but the axillary region was less dense than the rest; at the base, there was considerable reduction of diaphragmatic movements and the mass appeared lobulated.
Examination of the heart reveals nothing abnormal.
Liver and spleen of normal size.
No albumin or sugar in the urine.
No neurological disorders, normal tendon and ocular reflexes. No disorders of sensation, even within the skin lesions.
The testes are of normal consistency and retracted, the right is larger than the left.
This child was born at term and breast-fed; he was sick and treated at the hospital in Ulm for a year, and he was said to have had a left inguinal abscess at that time. It was around the age of 3 years that lesions appeared on the palms and soles; at the same time he started to lose teeth. He has been totally edentulous for two years. The child had mild rickets and did not walk until he was two years old. A tuberculin skin test was negative. Bordet-Wassermann's blood test was negative.
The girl weighs 13.6 kg; she is better nourished, even quite fleshy, especially in the thighs, where it is difficult to pinch the skin. She has significant sequelae of rickets: tibial curvature, slight beading of the ribs, widened epiphyses; she currently has impetigo, especially marked on the scalp, but with some lesions scattered on the trunk and on the left elbow, and impetigo is caused by louse infestation. Some inguinal nodes. No epitrochlear nodes.
The general examination is negative.
Neither sugar nor albumin.
Tuberculin skin test, negative.
Bordet-Wassermann reaction, negative.
She was breast-fed, never sick and walked late. The skin lesions of palms and soles appeared at around 2 years of age, after they were noticed in her brother. According to the mother, the brother passed on these lesions to his sister.
Family history
The parents of these two children are first cousins, they are healthy, and they have had 7 children: the eldest is 10 years old, the youngest 5 months old.
Neither the parents nor their relatives nor the other children have skin or dental lesions like those observed in the two children whom we present.
The other children are very healthy.
There has never been a miscarriage.
The two children that interest us were born in Ulm, one after the other, with no siblings between them.
The mother had no serious illnesses during her pregnancies with these two children.
In the presence of lesions on the palms and soles, we diagnosed keratoderma. Given the coincidence of absolutely identical lesions in the brother and sister, we only had to register the family history to reach the diagnosis of “familial symmetrical palmo-plantar keratoderma”, a condition in every way analogous to that observed by Ehlers on the island of Meleda, except for the endemic nature characterising the disease on that island.
The lesions on the knees were initially suggestive of psoriasis: scratching reveals the “candle-wax sign”, but without the other typical signs of psoriasis, and if we refer to the papers and descriptions of Ehlers and Neumann, we see that they reported keratoses on the knees in Meleda’s disease: they are also reported over the finger joints. The lesions that we have observed elsewhere than on the palms and soles do not refute our diagnosis; they seem to be an essential part of the clinical picture.
Will the two cases we have just described clarify the aetiology of familial keratoderma?
The occurrence of consanguinity already reported in such a case is noteworthy; this condition does not appear to be inherited or congenital.
Without evidence of chronic infection, syphilis can hardly be blamed for the appearance of these lesions. The history and investigations raise no suspicions.
The boy with his lymphadenopathy and suppurating glands, with his lung mass visible on X-rays, is very likely to have bacillary infection. However, his tuberculin test is negative and the lesions observed are not characteristic of tuberculosis. The possibility of a tuberculous background would be interesting here, but tuberculosis is not at all certain.
It is still necessary to consider endocrinopathy as a possible cause of this condition. Mr. Darier has already drawn attention to the possibility of this etiology in such cases, and the somewhat unusual condition of the skin, which is infiltrated especially in the girl’s thighs, is consistent with this hypothesis.
Finally, the striking coexistence of a dental disorder associated with skin lesions in these two children does not rule out the possibility of an endocrine disorder, specifically a problem with the parathyroids in which disordered calcium metabolism could explain the atrophic changes in the alveolar rim, tooth shedding and dental disease.
We therefore conclude with the diagnosis of “symmetrical familial palmar and plantar keratoderma” (Meleda’s disease). We would like to emphasize the interesting association with dental abnormalities possibly due, like the skin lesions, to an endocrinopathy. We note the parental consanguinity. Finally, we point out the palmoplantar hyperhidrosis, a major and early symptom for M. Lenglet.
M. DUBREUILH. - I think this is simply a case of palmar and plantar psoriasis.
M. DARIER. - Personally, I have no doubt that this is familial palmar and plantar keratoderma: the four extremities are affected symmetrically; moreover, there is a limited keratotic spot on one knee, as is not uncommon in such cases. The particular interest of this presentation is the dental disease in these children; it suggests that familial keratoderma may well be due to endocrine disorders and suggests treating patients with extracts of animal endocrine glands. Experience will show if this medication is useful.
DECLARATIONS
AcknowledgmentsThe authors thank Dr. Brigitte Roy-Geffroy (Société Française de Dermatologie), Sylvie Dorison, Altéa Swan, Alain Lecoq [Archives de l'Assistance publique-Hôpitaux de Paris (AP-HP)], Estelle Lambert (Archives Nationales) for providing historic documents and Prof Iain Chapple (School of Dentistry at the University of Birmingham, UK) for assistance with translation. The photos shown in Figure 6 are from the Private Collection of Y. Cukierman.
Authors’ contributionsAll the authors contributed to the concept, design, draft and revision of this manuscript.
Availability of data and materialsNot applicable.
Financial support and sponsorshipThis work was supported by the « Ministère de l’Enseignement Supérieur et de la Recherche » and the « Région Centre Val de Loire » (Project PIRANA, 2019-00134916).
Conflicts of interestAll authors declared that there are no conflicts of interest.
Ethical approval and consent to participateNot applicable.
Consent for publicationNot applicable.
Copyright© The Author(s) 2022.
REFERENCES
1. Toomes C, James J, Wood AJ, et al. Loss-of-function mutations in the cathepsin C gene result in periodontal disease and palmoplantar keratosis. Nat Genet 1999;23:421-4.
2. Shawli A, Almaghrabi Y, AlQuhaibi AS, Alghamdi Y, Aboud AM. A Mutation in Cathepsin C Gene Causing Papillon-Lefèvre Syndrome in a Saudi Patient: A Case Report. Cureus 2020;12:e6546.
3. Korkmaz B, Caughey GH, Chapple I, et al. Therapeutic targeting of cathepsin C: from pathophysiology to treatment. Pharmacol Ther 2018;190:202-36.
4. Papillon M, Lefevre P. Two cases of symmetrically familial palmar and plantar hyperkeratosis (Meleda disease) within brother and sister combined with severe dental alterations in both cases. Bull Soc Fr Dermatol Syphiligr 1924;31:82-7.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Korkmaz B, Seren S, Kara E, Moss C. The discovery of the Papillon-Lefèvre syndrome, a rare cathepsin C related lysosomal disease. Rare Dis Orphan Drugs J 2022;1:16. http://dx.doi.org/10.20517/rdodj.2022.26
AMA Style
Korkmaz B, Seren S, Kara E, Moss C. The discovery of the Papillon-Lefèvre syndrome, a rare cathepsin C related lysosomal disease. Rare Disease and Orphan Drugs Journal. 2022; 1(4): 16. http://dx.doi.org/10.20517/rdodj.2022.26
Chicago/Turabian Style
Korkmaz, Brice, Seda Seren, Elodie Kara, Celia Moss. 2022. "The discovery of the Papillon-Lefèvre syndrome, a rare cathepsin C related lysosomal disease" Rare Disease and Orphan Drugs Journal. 1, no.4: 16. http://dx.doi.org/10.20517/rdodj.2022.26
ACS Style
Korkmaz, B.; Seren S.; Kara E.; Moss C. The discovery of the Papillon-Lefèvre syndrome, a rare cathepsin C related lysosomal disease. Rare. Dis. Orphan. Drugs. J. 2022, 1, 16. http://dx.doi.org/10.20517/rdodj.2022.26
About This Article
Special Issue
Copyright
Data & Comments
Data

 Cite This Article 3 clicks
Cite This Article 3 clicks














Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.